Etrasimod: Uses, Interactions, Mechanism Of Action
Etrasimod is an orally administered drug used for the treatment of autoimmune and inflammatory diseases. It does so through counteracting specific cells in the immune system that are known to incite inflammation in the intestines. Etrasimod has been usually ingested in the form of a tablet and is taken orally. To control any side effect or any other concern that is associated with this medication, it is recommended to adhere to the healthcare provider’s directions.
USES
The primary use of etrasimod is in the treatment of ulcerative colitis (UC), a type of inflammatory bowel disease characterised by chronic inflammation of the colon. It is also being researched in moderate and severe UC to relieve bothersome signs and symptoms such as abdominal pain, diarrhoea, and bleeding. It has also been found that etrasimod has positive effects in inflammation, therefore deliver significant relief of UC symptoms and superior quality of life.
Due to its immune-modulating effects, etrasimod is being researched for other autoimmune conditions such as Crohn's disease, atopic dermatitis, and eosinophilic esophagitis. Its broad-spectrum impact on the immune system may make it suitable for a range of inflammatory diseases where traditional therapies are unable to help in curing the existing ailment.
MECHANISM OF ACTION
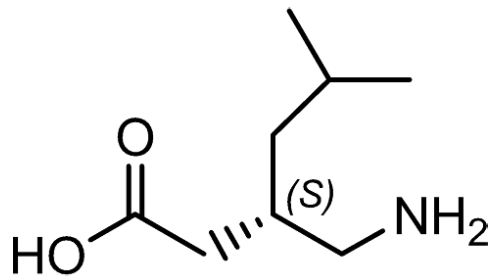
In autoimmune conditions, certain cells of the immune system are programmed to attack healthy tissue in the body, hence resulting in inflammation and destruction of body tissue. As an S1P receptor modulator, etrasimod immobilises lymphocytes in the lymph nodes, thereby denying them the opportunity to migrate to inflamed tissue. This targeted reduction in the mobility of lymphocytes is particularly useful in reducing inflammation in the tissues, for example in ulcerative colitis it reduces inflammation occurring in the intestines.
INTERACTIONS
As etrasimod is processed through the liver and metabolised by enzymes in the cytochrome P450 pathway, it has potential drug interactions that must be considered:
CYP Enzyme Modifiers: Medications that inhibit or induce CYP3A4 or CYP2C9 enzymes may affect the levels of etrasimod in the blood, either increasing the risk of side effects or reducing its effectiveness. The use of etrasimod requires frequent measuring of drug concentrations and dose titration when the patient receives these medicines simultaneously.
Immunosuppressive Agents: When combined with other immunosuppressive drugs, etrasimod can increase the risk of infections and immune-related complications. Combining it with potent immunosuppressants or biologics should be done cautiously and only under close supervision.
Heart Rate Modulators: Etrasimod may lower heart rate, especially at the initiation of therapy. Therefore, combining it with other drugs that also decrease heart rate may lead to bradycardia. Baseline heart rate monitoring and gradual dose titration can help mitigate this risk.
Live Vaccines: Since etrasimod is an immunosuppressive drug it can raise the risk of infections and immunological issues when used with other immunosuppressants. Its use along with other powerful immunosuppressive agents or biologics should be dual and under strict monitoring.
Some of the mild side effects include headache, nausea, abdominal pain, and flu-like symptoms including the cold. Etrasimod is expected to weaken the body’s immunity and increase its susceptibility to infections. For patents with a history of cardiac problems, they should be closely monitored, and dose titration may be advised to avoid imposing this risk. In occasional instances, there is liver enzyme increase, so monitoring of liver function can be performed before treatment and during it.
Other Recommended Products: https://www.enantilabs.com/aprocitentan-uses-interactions-mechanism-of-action.html